
You may notice something feels wrong with your vagina. You may feel extra tissue in your vagina that feels a little bit like a ball. Paired with pelvic and lower back discomfort, this may be a sign that you have a prolapsed bladder.
Other symptoms of bladder prolapse are:
- Difficulty urinating
- Feeling like you still have to ‘go’ even immediately after urination
- Tissue protruding from the vagina
- Heaviness or pressure in the vaginal area
- Frequent urinary tract infections
- Stress incontinence: leaking a little urine when sneezing, coughing, exercising or lifting heavy objects
- Painful intercourse
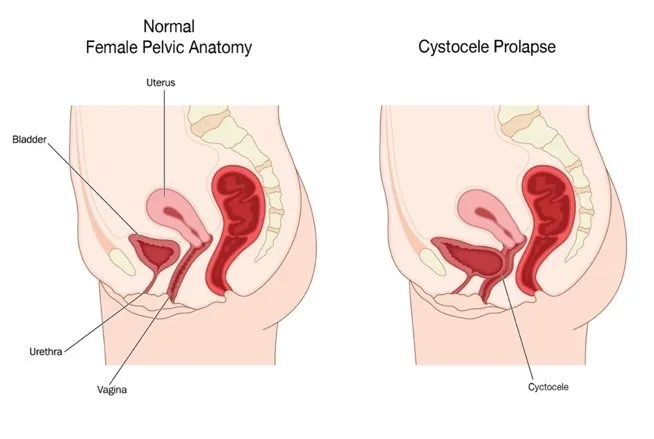
In women, the pelvic floor muscles work in conjunction with the front wall of the vagina to support the bladder, a hollow organ that fills up with urine, signalling when it’s time to go. When the pelvic floor muscles surrounding the bladder weaken or loosen, the bladder is no longer supported, causing it to slouch against the vagina and creating an obstruction or bulge in the vaginal cavity.
Prolapsed bladders in women are commonly associated with menopause. The lower levels of oestrogen associated with menopause can cause the vaginal walls to weaken. If they deteriorate enough, the bladder is no longer supported and can fall into the vagina. This can cause urinary problems such as stress incontinence.
Other risk factors for bladder prolapse are:
-
Childbirth
-
Surgery, such as a hysterectomy
-
Excessive strain on the pelvic floor from things like long-term constipation, lifting heavy objects or weight gain
-
Chronic coughing (or other lung problems)
Bladder prolapse is separated into four grades, each characterised by how far the bladder has sunk into the vagina.
-
Grade 1 (mild): Only a small portion of the bladder droops into the vagina
-
Grade 2 (moderate): The bladder droops enough to be able to reach the opening of the vagina
-
Grade 3 (severe): The bladder protrudes from the body through the vaginal opening
-
Grade 4 (complete): The entire bladder protrudes completely outside the vagina
The good news is that bladder prolapse is rarely a life-threatening condition. Most cases can be corrected non-surgically. Your treatment plan will depend largely on the grade of prolapse you have.
If surgery is not needed, here are some at-home remedies for bladder prolapse:
-
Pelvic floor exercises. The pelvic floor is a system of muscles, ligaments and nerves that creates a basket of support for our bladder. Fitting these exercises into your routine can been pretty straightforward. As you’re sitting at your desk, flex and release the muscles used to hold in urine. Do this at least three times a day and you’ll start seeing results.
-
Lifestyle changes.It may be recommended that you avoid lifting heavy objects. If you have chronic constipation, remedies to correct this are also recommended.
-
Pessary. A pessary is a device inserted into the vagina in order to provide support for the bladder. Pessaries require regular removal and cleaning in order to avoid infection. Depending on what kind of pessary you are fitted with, removal is performed by a doctor or at home. Some women find pessaries uncomfortable or find that they easily fall out.
-
Oestrogen replacement therapy. Oestrogen, which a woman’s body stops producing after menopause, can prompt the body to strengthen the muscles around the vagina and bladder. This can correct bladder prolapse in some mild to moderate cases. However, hormone therapy isn’t for everyone. Consult your doctor.
If you have severe bladder prolapse, surgery may be required. During surgery, a mesh support is inserted into the vaginal wall and the bladder’s position is corrected. This can be performed under general, regional or local anaesthetic.
Bladder prolapse can only be diagnosed by a health care provider. If you are experiencing symptoms of bladder prolapse, consult your GP. Together you can discuss a treatment plan.
* If you are going through menopause or experiencing bladder leaks, always make sure to consult your doctor or a health specialist for these medical conditions.





